Cutaneous Vasculitis: Understanding Reddened Skin Bumps and Beyond

Cutaneous vasculitis is like a tiny plumbing system gone haywire in your skin. Instead of blood flowing smoothly, inflammation clogs up the small vessels, causing red splotches, bumps, and even ulcers. It can come from various triggers, like infections, medications, or even autoimmune issues. While sometimes it’s a solo act, it can also be a sign of a bigger problem affecting your internal organs.
Cutaneous Vasculitis: Signs and Symptoms
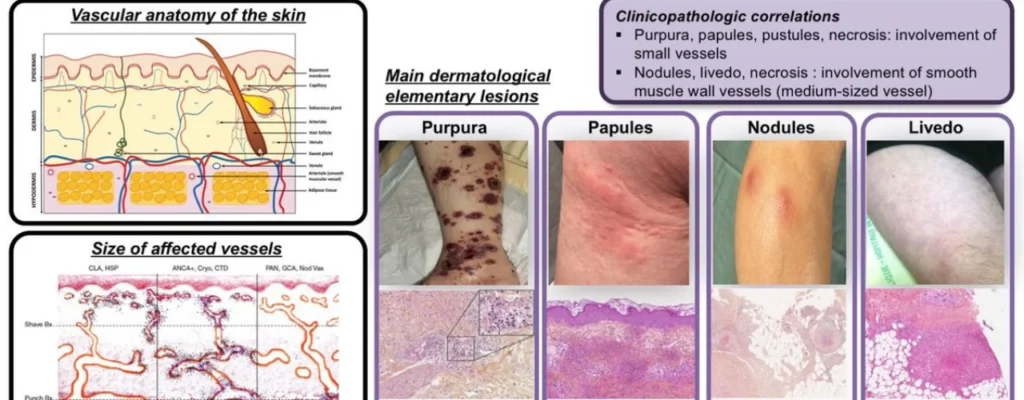
Cutaneous vasculitis primarily affects the small and medium-sized blood vessels in your skin and underlying tissue, leading to a variety of skin lesions and sometimes general symptoms. Here’s a breakdown of the most common signs and symptoms:
Skin Lesions:
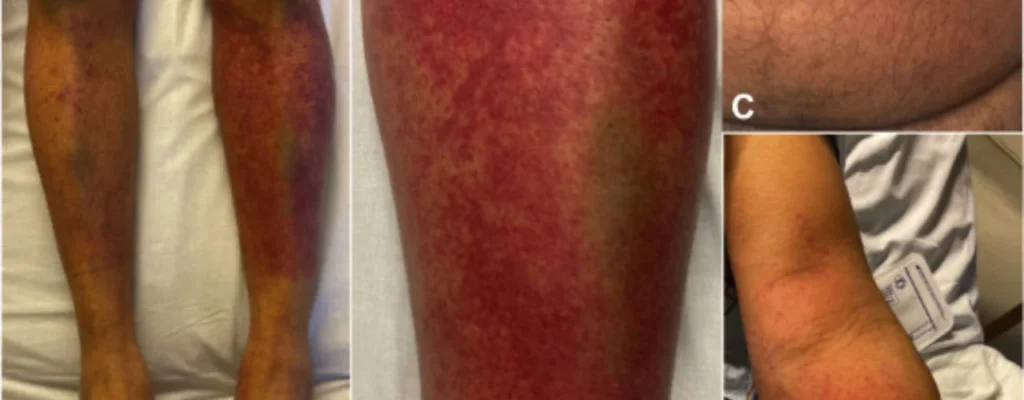
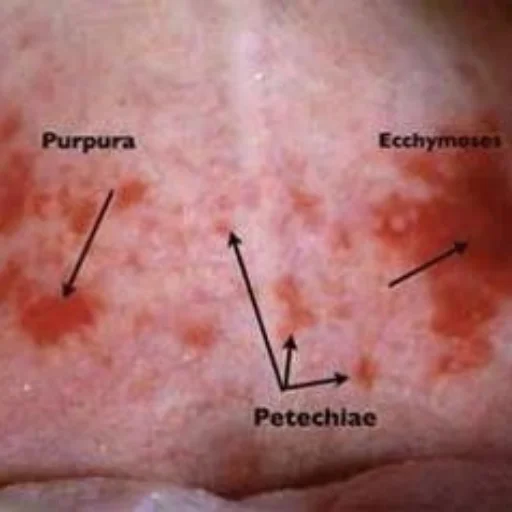
- Palpable purpura: Raised, palpable reddish-purple patches or bumps, often occurring on the legs, buttocks, and lower back. These can be tender and may leave scars after healing.
- Petechiae: Tiny, flat, non-blanching reddish-brown spots caused by bleeding under the skin, similar to pinpoint bruises. They usually appear on the lower extremities but can occur anywhere.
- Urticaria (hives): Raised, itchy, welts that can range in size and shape, often appearing in clusters and changing location over time.
- Ulcers: Open sores that develop due to tissue damage from the inflammation. These can be painful and slow to heal, potentially leaving scars.
- Livedo reticularis: A net-like or lace-like pattern of reddish-blue discoloration on the skin, often most visible on the legs. It can be transient or persistent.
- Nodules: Firm, raised bumps or lumps on the skin, typically larger than petechiae or purpura. They can be tender and may ulcerate in severe cases.
General Symptoms:
- Fever: A common symptom, especially if the vasculitis is part of a systemic disease.
- Arthralgias: Joint pain and stiffness, particularly in the knees, ankles, and wrists.
- Other organ involvement: Depending on the type and severity of vasculitis, involvement of other organs like the kidneys, lungs, or nervous system is possible. This can lead to various symptoms like bloody urine, difficulty breathing, or neurological problems.
It’s important to note that:
- The specific type and severity of cutaneous vasculitis determine the exact signs and symptoms experienced.
- Some people may only have mild skin involvement, while others may have more extensive lesions and general symptoms.
- If you experience any of these signs or symptoms, especially new or rapidly worsening ones, consult a healthcare professional promptly for diagnosis and proper management.
Remember, early diagnosis and treatment are crucial for preventing complications and ensuring optimal outcomes.
Classification of Cutaneous Vasculitis: A Look into the Different Types
Cutaneous vasculitis is a diverse group of disorders characterized by inflammation of blood vessels in the skin and underlying tissue. Classifying these disorders helps guide diagnosis, treatment, and understanding of their potential outcomes. Here’s a breakdown of the different types of cutaneous vasculitis:
1. Capillaritis:
- Affects the smallest blood vessels in the skin.
- Symptoms: palpable purpura (raised, reddish-purple bumps), petechiae (flat, pinpoint bruises), and sometimes ulcers.
- Types:
- Progressive pigmented purpura: most common form, often affects lower legs, tends to leave scars.
- Itching purpura: itchy, burning lesions, often triggered by medications or infections.
- Pigmented purpuric lichenoid dermatosis: papules and nodules with purpuric borders, associated with chronic viral infections like hepatitis C.
- Purpura annularis telangiectodes: ring-shaped lesions with central red spots, sometimes related to autoimmune diseases.
- Capillaritis in association with contact allergy: caused by allergic reaction to chemicals or metals.
- Lichen aureus: small, yellow-red papules with central crusts, usually on legs, associated with chronic venous insufficiency.
2. Small Vessel Vasculitis:
- Affects slightly larger vessels than capillaritis.
- Types:
- Idiopathic, drug or infection-induced cutaneous small vessel vasculitis (hypersensitivity vasculitis): most common type, often triggered by medications or infections, typically self-limited.
- Henoch-Schönlein purpura: affects children, with joint pain, abdominal pain, and kidney involvement in addition to skin lesions.
- Acute hemorrhagic edema of infancy: rare, affects very young children, with fever, swelling, and skin lesions.
- Urticarial vasculitis: wheals (hives) with central hemorrhagic spots, associated with infections or autoimmune diseases.
- Exercise-induced vasculitis: triggered by exercise, with burning, itching, and swelling after exertion.
- Erythema elevatum diutinum: chronic, with papules and nodules on hands and forearms, sometimes associated with internal organ involvement.
- Lymphocytic thrombophilic arteritis: rare, affects small arteries, with livedo reticularis (net-like discoloration) and skin ulcers.
- Malignant atrophic papulosis (Degos): rare, with small, white papules that evolve into atrophic scars, mostly on trunk and extremities.
- Cryoglobulinemia: associated with abnormal blood proteins that precipitate in the cold, with skin lesions, fatigue, and joint pain.
- Recurrent cutaneous necrotizing eosinophilic vasculitis: rare, with painful ulcers and nodules, particularly on legs, associated with eosinophils (a type of white blood cell).
- ANCA-associated vasculitis:
- Microscopic polyangiitis: affects small vessels in various organs, with kidney and lung involvement along with skin lesions.
- Eosinophilic granulomatosis with polyangiitis / Churg-Strauss: affects small vessels, with asthma, lung infiltrates, and skin lesions.
- Granulomatosis with polyangiitis (Wegener’s granulomatosis): affects small and medium vessels, with respiratory tract, kidney, and skin involvement.
- Lymphomatoid granulomatosis: rare, with granulomas (inflammatory nodules) in skin and internal organs, associated with EBV infection.
3. Medium Vessel Vasculitis:
- Affects medium-sized arteries and veins.
- Types:
- Cutaneous polyarteritis nodosa: involves small and medium vessels, with nodules on skin and livedo reticularis, can affect internal organs.
Cutaneous Vasculitis Diagnosis:
Diagnosing cutaneous vasculitis involves a two-pronged approach: excluding other causes and confirming the vasculitis itself. Here’s a breakdown of the steps involved:
1. Excluding Other Causes:
- Clinical History and Physical Examination: This initial step aims to identify any potential triggers or conditions that might mimic vasculitis symptoms, such as recent drug use, infections, or other vasculitic syndromes affecting internal organs.
- Routine Tests: These include checks for:
- Blood: Anemia, platelet count, kidney function (serum creatinine), inflammation markers (erythrocyte sedimentation rate, C-reactive protein).
- Urinalysis: Presence of blood, protein, or red blood cell casts, which could indicate kidney involvement.
- Chest X-ray: To rule out lung problems like pneumonia or hemorrhage.
2. Confirming Cutaneous Vasculitis:
- Skin Biopsy: Crucial for diagnosis, ideally within 24-48 hours of symptom onset. A deep punch or excision biopsy is preferred to analyze both small and medium-sized vessels. A shave biopsy is usually insufficient.
- Histological Examination: If the biopsy reveals the following, it confirms vasculitis:
- Inflammation infiltrating the vessel wall: Damage and destruction of the vessel structure.
- Fibrin deposition within and around the vessels: Evidence of blood clotting and tissue damage.
- Extravasation of red blood cells: Leakage of blood cells from damaged vessels.
- Nuclear debris (leukocytoclasis): Breakdown of white blood cells within the vessel wall.
- Direct Immunofluorescence Staining: This further assesses immune system involvement by detecting antibody or complement deposition around the vessels. Different patterns can suggest specific types of vasculitis.
- IgA deposition: Suggests kidney, joint, or gastrointestinal involvement.
- IgM or IgG deposition: Seen in cryoglobulinemic vasculitis or rheumatoid arthritis.
Additional Tests:
Based on the initial findings, specific tests might be ordered to identify the underlying cause of the vasculitis, such as:
- Cryoglobulins: Proteins that precipitate in the cold, associated with cryoglobulinemic vasculitis.
- Antineutrophil cytoplasmic antibodies (ANCA): Autoantibodies targeting white blood cells, seen in some vasculitic syndromes.
- Hepatitis B and C antibodies: Viral infections can trigger vasculitis.
- C3 and C4 complement levels: These proteins aid the immune system, and their levels can be affected in vasculitis.
- Rheumatoid factor: Marker for rheumatoid arthritis, which can sometimes present with vasculitis-like skin lesions.
- Blood cultures: Rule out infections as a potential cause.
- Serum and urine protein electrophoresis: Detect abnormal protein production in the blood or urine, potentially indicating underlying conditions.
Remember: Early and accurate diagnosis is crucial for determining the appropriate treatment and preventing potential complications.
Treatment of Cutaneous Vasculitis:
The approach to treating cutaneous vasculitis depends on several factors, including the identified cause, severity of symptoms, and extent of the disease. Here’s a breakdown of the different steps involved:

1. Addressing the Underlying Cause:
This is the first line of treatment if a specific trigger or condition is identified, such as hepatitis C causing cryoglobulinemia. By treating the underlying cause, the vasculitis symptoms may resolve or improve significantly.
2. Initial Treatment for Skin-Limited Disease:
If no trigger is found and the vasculitis is confined to the skin, the approach is usually conservative and aims to control the inflammation and alleviate symptoms. Here are some common medications used:
- Colchicine: This medication has anti-inflammatory properties and can be effective in mild cases.
- Hydroxychloroquine: This medication also has anti-inflammatory and immune-suppressing effects, often used for longer-term control.
- Dapsone: This medication has anti-inflammatory and antibiotic properties, sometimes used in combination with other treatments.
- Low-dose corticosteroids: Short-term use of oral corticosteroids can provide quick relief from inflammation and pain, but prolonged use is not recommended due to potential side effects.
3. Escalating Treatment for More Severe Cases:
In more severe cases, especially those with extensive skin involvement, ulceration, or requiring long-term corticosteroid use, stronger immunosuppressant medications may be necessary. These drugs suppress the immune system and reduce inflammation, often used in combination with the initial options mentioned above. Examples include:
- Azathioprine: This medication suppresses the immune system and can be effective for controlling severe or persistent vasculitis.
- Methotrexate: Similar to azathioprine, this medication suppresses the immune system and can be used in severe cases.
4. Additional Supportive Measures:
Apart from medications, certain supportive measures can help manage the symptoms and improve overall well-being:
- Wound care: For open sores or ulcers, proper cleaning and dressing are crucial to prevent infection and promote healing.
- Pain management: Over-the-counter pain relievers or prescription medications can be used to manage pain.
- Sun protection: Protecting the skin from sun exposure can help prevent worsening of lesions and scarring.
- Emotional support: Living with a chronic condition can be challenging, so seeking emotional support from family, friends, or a therapist can be beneficial.
Remember: The specific treatment plan for cutaneous vasculitis will be individualized based on each patient’s unique situation. It’s crucial to consult with a healthcare professional to receive proper diagnosis, discuss treatment options, and monitor the disease progression.
Final Conclusion:
Cutaneous vasculitis can arise from various causes, including infections, medications, autoimmune issues, and even unknown factors. Identifying the underlying trigger is crucial for proper management.
The disease can manifest differently, ranging from mild skin rashes with minimal discomfort to severe ulcerations and even internal organ involvement in some cases. If you experience any suspicious skin lesions or suspect vasculitis, consult doctor for proper diagnosis and personalized guidance.
Derma and Dental Clinic:
Derma & Dental Clinic stands out with its team of experienced doctors backed by scientific evidence in their chosen fields. Their diverse range of medical-grade procedures offer tailored solutions for various skin and dental needs. You can confidently book your consultation online or by phone and embark on your journey towards healthier skin and a radiant smile.
Location: Bahria Town, Lahore
Specialties: Dermatology and Dental Care
Website: derma.pk
For Appointment:
- Online at Dermatology.pk
- WhatsApp: +923205999650
- Phone: 03041115000