PCOS: Unveiling the Skin, Hair, and Hormonal Imbalance

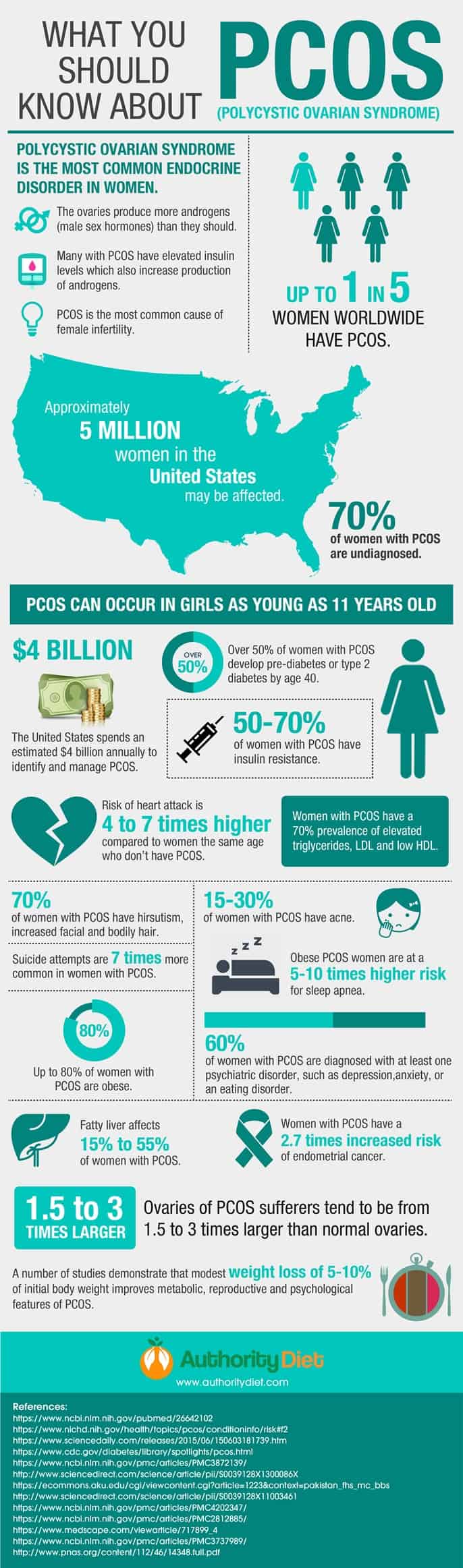
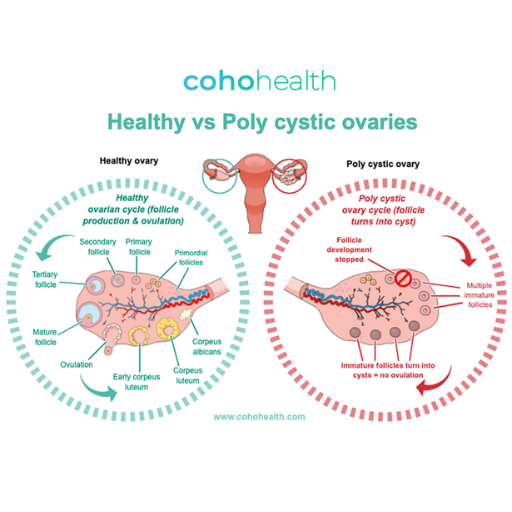
Polycystic Ovary Syndrome (PCOS) is a common hormonal disorder affecting women of childbearing age. It is characterized by a complex interplay of hormonal imbalances, irregular periods, and the presence of numerous small cysts on the ovaries. While the exact cause of PCOS remains unknown, understanding its symptoms, PCOS skin, hair, and hormonal imbalance, potential complications, and available treatment options can empower women to manage their health effectively.
Causes of PCOS:
While the exact cause of PCOS remains unknown, several factors are believed to contribute to its development:
1. Genetics: PCOS appears to have a strong hereditary component. Women with a family history of PCOS are at an increased risk of developing the condition.
2. Insulin resistance: This is a condition where your body’s cells do not respond properly to the hormone insulin, which regulates blood sugar levels. Insulin resistance can lead to increased production of androgens, male hormones, by the ovaries. High androgen levels can interfere with ovulation and contribute to other PCOS symptoms.
3. Inflammation: Low-grade chronic inflammation is thought to play a role in PCOS. This inflammation can further contribute to insulin resistance and androgen production.
4. Environmental factors: Studies suggest that certain environmental factors, such as exposure to endocrine-disrupting chemicals (EDCs), may also contribute to the development of PCOS.
5. Vitamin D deficiency: Some research suggests a potential link between vitamin D deficiency and PCOS, although further studies are needed to confirm this association.
6. Gut microbiota: The balance of gut bacteria may also play a role in PCOS. Studies have shown that women with PCOS have different gut microbiota profiles compared to women without the condition.
It is important to note that no single factor is solely responsible for causing PCOS. It is likely a complex interplay of these and potentially other unknown factors that contribute to its development.
Here are some resources where you can learn more about the causes of PCOS
- National Institute of Child Health & Human Development: https://www.nichd.nih.gov/health/topics/pcos
- Mayo Clinic: https://www.mayoclinic.org/diseases-conditions/pcos/symptoms-causes/syc-20353439
- PCOS Foundation: https://www.pcosaa.org/
Symptoms of PCOS:
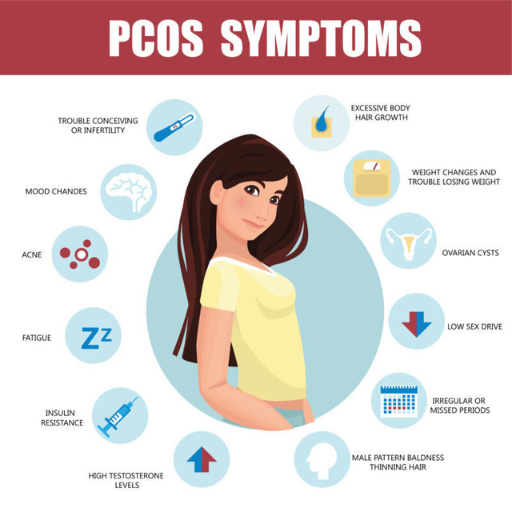
- Irregular periods or no periods at all
- Excess hair growth on the face, chest, or back (hirsutism)
- Acne or oily skin
- Weight gain or difficulty losing weight
- Thinning hair or hair loss
- Difficulty getting pregnant
- Fatigue
Diagnosing Polycystic Ovary Syndrome (PCOS)
There is no single test for PCOS, but doctors typically rely on a combination of three key criteria to diagnose the condition:
1. Irregular ovulation: This is typically indicated by irregular periods or a complete absence of periods (amenorrhea). A normal menstrual cycle is 21-35 days, and irregular periods are defined as cycles that are longer than 35 days, shorter than 21 days, or occur at unpredictable intervals.
2. Signs of increased androgen levels: These can include:
Excess hair growth (hirsutism): This is the growth of coarse, dark hair on the face, chest, back, abdomen, or buttocks in a pattern typically seen in men.
Acne: This is caused by the overproduction of oil by the skin glands, which can lead to pimples, blackheads, and cysts.
Male-pattern baldness: This is the thinning of hair on the scalp in a pattern typically seen in men.
Blood tests: These can measure the levels of hormones like testosterone and androstenedione, which are considered male hormones.
3. Polycystic ovaries: This is characterized by the presence of many small cysts (fluid-filled sacs) on the ovaries. These cysts can be detected by a pelvic ultrasound.
Here are the steps involved in diagnosing PCOS:
- Medical history: Your doctor will ask about your symptoms, menstrual history, family history, and any medications you are taking.
- Physical exam: This may include checking for signs of excess hair growth, acne, and changes in skin texture.
- Blood tests: These can measure your levels of hormones like testosterone, androstenedione, follicle-stimulating hormone (FSH), luteinizing hormone (LH), and fasting insulin.
- Pelvic ultrasound: This can help identify the presence of cysts on your ovaries.
It is important to note that not all women with PCOS will exhibit all three of these diagnostic criteria. Some women may only meet two of the criteria, while others may have all three. Ultimately, the diagnosis of PCOS is a clinical judgment made by your doctor based on your individual symptoms and test results.
Here are some resources where you can learn more about the diagnosis of PCOS Impact on skin, hair and hormonal imbalance:
- National Institute of Child Health & Human Development: https://www.nichd.nih.gov/health/topics/pcos
- Mayo Clinic: https://www.mayoclinic.org/diseases-conditions/pcos/symptoms-causes/syc-20353439
- PCOS Foundation: https://www.pcosaa.org/
Potential Complications of PCOS:
- Type 2 diabetes
- High cholesterol
- High blood pressure
- Sleep apnea
- Endometrial cancer
- Depression and anxiety
Treatment options for PCOS:
While there is no cure for PCOS, there are several effective treatments available to manage the symptoms and reduce the risk of long-term complications. The best treatment approach for you will depend on your individual symptoms and goals.
Here are some of the main treatment options for PCOS:
Lifestyle changes:
- Diet: Eating a healthy diet, such as a Mediterranean or DASH diet, can help improve insulin sensitivity, regulate periods, and reduce the risk of weight gain. This typically involves focusing on whole grains, fruits, vegetables, lean protein, and healthy fats while limiting processed foods, sugary drinks, and excessive amounts of saturated and unhealthy fats.
- Exercise: Regular physical activity, at least 150 minutes of moderate-intensity exercise or 75 minutes of vigorous-intensity exercise per week, can also improve insulin sensitivity, regulate periods, and promote weight loss. Aiming for at least 30 minutes of moderate-intensity exercise most days of the week is a good starting point.
- Weight management: If you are overweight or obese, losing even a small amount of weight (5-10%) can significantly improve your symptoms.
Medications:
- Hormonal birth control: Oral contraceptives, such as birth control pills or the progesterone-only pill, can help regulate your menstrual cycle, reduce acne, and decrease hair growth.
- Metformin: This medication can improve insulin sensitivity and regulate ovulation. It can also help with weight loss and reduce the risk of type 2 diabetes.
- Anti-androgen medications: These medications can help block the effects of androgens and reduce symptoms like acne and excess hair growth.
- Clomiphene citrate: This medication can stimulate ovulation and is often used to help women with PCOS conceive.
- Gonadotropins: These are injectable medications that can be used to stimulate ovulation in women who do not respond to clomiphene citrate.
Surgery:
- Laparoscopic ovarian drilling: This is a minimally invasive surgical procedure that can be used to restore ovulation in women with PCOS who are not responding to other treatments.
Other therapies:
- Inositol: This supplement may help improve insulin sensitivity and regulate ovulation.
- N-acetylcysteine (NAC): This supplement may help improve symptoms like acne and hirsutism.
- Vitamin D supplementation: If you are vitamin D deficient, supplementing with vitamin D may help improve your symptoms.
Here are some additional resources where you can learn more about the treatment of PCOS skin, hair, and hormonal imbalance:
- National Institute of Child Health & Human Development: https://www.nichd.nih.gov/health/topics/pcos
- Mayo Clinic: https://www.mayoclinic.org/diseases-conditions/pcos/diagnosis-treatment/drc-20353443
- PCOS Foundation: https://www.pcosaa.org/
It is important to work with your doctor to develop a personalized treatment plan that is right for you. Remember, PCOS is a lifelong condition, but with proper management, you can live a healthy and fulfilling life.
PCOS and its Impact on Skin, Hair, and Hormonal Imbalance
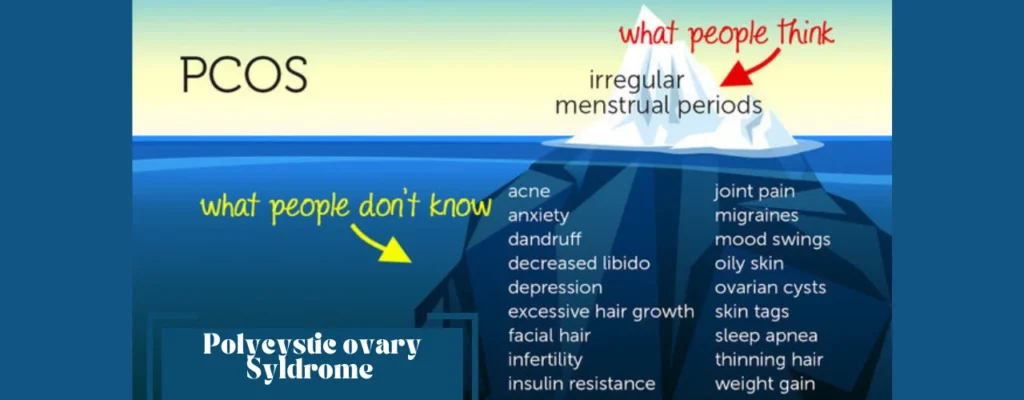
Polycystic Ovary Syndrome (PCOS) is a complex hormonal disorder affecting millions of women worldwide. It disrupts the delicate hormonal balance, leading to various symptoms, including those affecting skin, hair, and overall well-being. This article explores the intricate relationship between PCOS and its effects on these aspects.
Understanding Hormonal Imbalance in PCOS:
PCOS disrupts the normal hormonal equilibrium in women, affecting:
- Androgens: These male hormones, typically present in small amounts in women, are overproduced in PCOS, leading to imbalances.
- Insulin: This hormone regulates blood sugar levels. In PCOS, cells often resist insulin, leading to elevated insulin levels.
- FSH and LH: These hormones regulate ovulation. In PCOS, their levels are often imbalanced, disrupting the ovulation process.
Skin and Hair Changes:
The hormonal imbalances in PCOS can manifest in various skin and hair changes, including:
Skin:
- Acne: Increased androgen levels stimulate oil glands, causing acne breakouts on the face, chest, and back.
- Oily Skin: The overactive oil glands contribute to oily skin, making it prone to breakouts.
- Hirsutism: Excessive hair growth on the face, chest, back, and abdomen occurs due to increased androgens.
- Acanthosis Nigricans: This condition causes dark, velvety patches on the neck, armpits, and groin, often associated with insulin resistance.
- Skin Tags: Small, fleshy skin growths may appear on the neck, armpits, and groin.
Hair:
- Hair Loss: PCOS can cause thinning hair and hair loss on the scalp, often resembling male-pattern baldness.
- Changes in Hair Texture: Hair may become dry, brittle, and more prone to damage due to hormonal changes.
Impact on self-esteem:
The skin and hair changes associated with PCOS can significantly impact a woman’s self-esteem and confidence. Acne, excessive hair growth, and hair loss can be emotionally distressing and lead to feelings of self-consciousness and social anxiety.
Management strategies:
Fortunately, several strategies can help manage the skin and hair manifestations of PCOS:
- Medications: Certain medications, such as birth control pills, anti-androgen medications, and metformin, can help regulate hormones and alleviate skin and hair issues.
- Skincare routine: Using gentle cleansers, oil-free moisturizers, and topical acne treatments can help manage oily skin and acne.
- Hair removal: Various hair removal methods, such as shaving, waxing, laser hair removal, and electrolysis, can help manage unwanted hair growth.
- Scalp care: Using a gentle shampoo and conditioner, avoiding heat styling, and scalp massages can promote healthy hair growth.
- Nutritional support: Eating a balanced diet rich in fruits, vegetables, and whole grains can help regulate blood sugar levels and improve overall skin and hair health.
- Stress management: Stress can worsen PCOS symptoms, including skin and hair problems. Practicing stress-management techniques like yoga, meditation, and deep breathing can be beneficial.
- Support groups: Connecting with other women who understand the challenges of PCOS can provide invaluable emotional support.
Consequences of Hormonal Imbalance:
Beyond skin and hair changes, the hormonal imbalances in PCOS can lead to various health consequences, including:
- Irregular Menstrual Cycles: This is the most common symptom, with women experiencing infrequent, heavy, or absent periods.
- Infertility: The disrupted ovulation process can make it challenging to conceive naturally.
- Hirsutism: Excessive hair growth on the face, chest, back, and abdomen is a common manifestation of increased androgen levels.
- Acne: Oily skin and acne are frequent problems due to the overactivity of oil glands stimulated by androgens.
- Weight Gain and Difficulty Losing Weight: Insulin resistance can contribute to weight gain and make it challenging to lose weight.
- Metabolic Syndrome: This cluster of risk factors, including high blood pressure, high cholesterol, and high blood sugar, increases the risk of developing type 2 diabetes and heart disease.
Managing the Impact of PCOS:
While PCOS is a lifelong condition, several strategies can help manage its symptoms and address the underlying hormonal imbalance:
Lifestyle Modifications:
- Diet: Eating a balanced diet with fruits, vegetables, and whole grains improves insulin sensitivity and regulates hormone production.
- Exercise: Regular physical activity aids in weight management and improves overall health.
- Stress Management: Techniques like yoga and meditation help reduce stress, which can worsen PCOS symptoms.
Medications:
- Birth control pills: These regulate menstrual cycles and reduce androgen levels.
- Anti-androgen medications: These manage unwanted hair growth.
- Metformin: This medication improves insulin sensitivity in women with PCOS.
Complementary Therapies:
- Acupuncture and yoga: These practices offer additional benefits in managing PCOS symptoms.
Working with a Healthcare Team:
- Consult a doctor specializing in PCOS and a registered dietitian for a personalized treatment plan and ongoing monitoring.
Conclusion:
PCOS’s impact extends beyond irregular periods, affecting skin, hair, and overall health. Understanding the hormonal imbalances and their consequences empowers women with PCOS to take control of their well-being. Through a combination of lifestyle modifications, medical interventions, and support from healthcare professionals, women with PCOS can effectively manage their symptoms and live fulfilling lives.
PCOS skin hair and hormonal imbalance